Everyone recovers at different rates after surgery. It depends on the surgical procedure you had, your health prior to the surgery, as well as many personal factors.
It is important that you listen to your body, follow the directions of your health care team, and actively work on getting better.
There are a number of things that your health care team may ask you to do during this time, which will help you to get better. This can include walking, or sitting on the edge of your bed, very soon after surgery, and deep coughing and breathing exercises. Nurses will also be very busy following the care instructions from your surgeon. This may include things like changing your bandages, giving you pain medication and antibiotics, inserting a catheter, and catering for any special requirements.
Your discharge process will begin once your health care team are assured that you are amply recovered.
Depending on your level of recovery, you could be discharged to another health care facility to continue your rehabilitation until you are well enough to go home.
When you are able to return to your home the medical staff will provide a list of discharge instructions specific to your needs, including specific instructions about medication and wound care. It is important that you share this information with your GP, and work with them to follow these instructions closely.
Some of the important parts of the Recovery phase in your surgery journey are:
Pain relief
Pain is our body’s way of telling us that something is wrong.
You may have pain following surgery. This pain should go away after the area operated on has healed. After your surgery, you will be given pain relief as you need it. The most common way to control acute pain is to take pain relieving medicines.
You will be asked to rate your pain when you are resting and moving. Pain is assessed regularly after your surgery.
You will be asked by your nurse or doctor to score how bad your pain is while you are lying still and, more importantly, when you move about or cough. The hospital staff may use a pain scale to help assess the amount of pain you have. You need to give your pain a rating out of 10, which best represents your pain.
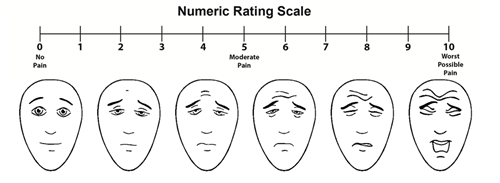
You will give a number between 0 (no pain) and 10 (worst possible pain). This describes how much pain you feel in your surgery site or wound. The pictures below will help you rate your pain.
Image used with permission. Faces Pain Scale – Revised, ©2001, International Association for the Study of Pain.
You will be asked to do this regularly to help your nurses and doctors choose the best medicine and dose for you. Although we would like to take away all the pain and discomfort, sometimes pain cannot be removed completely. Our aim is to make you as comfortable as possible. This especially includes when moving around and performing activities.
Do not wait until the pain becomes very bad. If pain is treated early the medicine can make it go away quickly. Tell your nurse when you need pain relief or if you did not get better after taking the medicine.
Is pain relief important?
Yes. As well as making you more comfortable, good pain relief may help in faster recovery, even for those who have major surgery.
Good pain control can help you:
- Be more comfortable after your surgery
- Get well faster. With less pain, you can start to walk, do your breathing exercises and get your strength back more quickly
- Improve your results. People whose pain is well controlled do better after surgery with less problems
Pain can almost always be relieved, and a variety of methods are available. These include:- Tablets
- Occasional injections (needles)
- Patient Controlled Analgesia (PCA)-small doses of pain medicine controlled by you via a drip
- Local anaesthetic given near your wound that stops the feeling of pain
- Epidural analgesia given into your back that blocks the pain over your wound
Regular Paracetamol is often the best treatment for mild to moderate pain. For more severe acute pain, stronger medicines are given. Morphine, Fentanyl or Oxycodone are examples. They are also called opioids.
If you have wound pain we may give you anti-inflammatory drugs. By adding 2 or more medicines that work in different ways, smaller amounts of the strong opioid medicine may be needed. You should always ask your doctor what medicine is safest after surgery.
The aim of good pain control is pain relief without unpleasant side effects.
Anaesthetists are doctors who look after your medicine during your surgery. They also specialise in pain relief. The Acute Pain Service is part of the Anaesthetic Department.
An Anaesthetist and a nurse may see you at least once a day from the Acute Pain Service as well as the doctors and nurses who provide your regular ward care.
Leg stockings
Before and after surgery the nurses might help you put on tight fitting stockings. These help to keep blood circulating while you are having your surgery. These stockings are fitted to reduce the threat of a blood clot forming in your legs. We call these clots Deep Vein Thrombosis or DVT.
There are 3 main triggers of blood clots:
- Not moving for long periods of time. For example, having to stay on bed rest, or travelling on longs trips without getting up and walking around.
- A hospital stay for an extended time. More than 60% of all blood clots are caused by this.
- Surgery, especially hip and knee surgery and surgery for cancer, puts a patient at higher risk.
There are also some other risk factors:
- Being overweight can increase the chance of developing a clot. You should try to stay active before surgery.
- Cigarette smoking. You should avoid cigarettes.
- Using oestrogen based medicines like the oral contraceptive pill and hormone replacement therapy. Talk to your local doctor before any surgery.
- Being pregnant or having recently given birth
- Older age
- Heart disease
- A family history of blood clots
If you have been given anti-blood clot stockings, wear them day and night while you are in hospital. You can take them off when you have a shower or bath. Some patients will not be provided with stockings as they can make lower leg conditions worse. Please ask your nurse or doctor if you should be wearing stockings.
Some patients will have a special lower leg (calf) compression device fitted while they are having surgery. This machine will squeeze the feet and lower legs to help keep blood circulating while in surgery and in the days afterwards.
The symptoms of a Deep Vein Thrombosis (DVT) may include:
- Pain and tenderness in the leg
- Pain on extending the foot
- Swelling of the lower leg, ankle and foot
- Skin that is red and warm
It is very important that you tell us if you notice any of these symptoms.
Going home
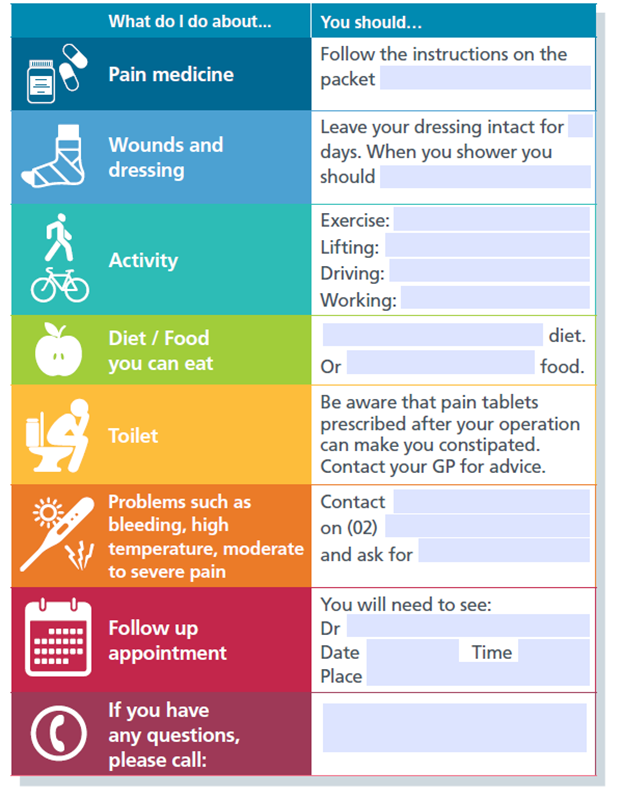
Before you go home, a nurse will help you complete the following information. If you had a day procedure a Nurse may telephone you the next day to check how you are doing.
Concerns after surgery
After your surgery you will recover and head home. You must have someone drive you home and stay with you the night after your surgery (if you are discharged).
This is for your own safety as you may be lightheaded and drowsy. Your ability to do tasks may be affected. A small amount of anaesthetic may still be in your body.
If you don’t have a family member or friend able to pick you up and stay with you please tell the hospital staff before your surgery. We want you to have your surgery but we also want you to be safe afterwards.
You might also need someone to help you in the days and weeks after surgery. This could be a family member, friend or even a neighbour.
Your doctor will tell you when you can get back to activities such as driving or exercise.
If you feel unwell, have severe pain or notice something doesn’t look quite right: you need to see a doctor. This could be your local doctor, specialist or you might need to go to your nearest emergency department.
Go to your nearest Emergency Department or dial 000 if you experience:
- Uncontrollable bleeding
- Chest pain or tightness
- Breathing difficulty
- Change in alertness/difficulty in waking
- Sudden onset of weakness, numbness or paralysis of the face, arm or leg
- Sudden collapse or unexplained fall
- Unexplained fitting in adults
- Blood in vomit, when coughing or with bowel movements
IMPORTANT: DO NOT DRIVE YOURSELF TO THE EMERGENCY DEPARTMENT
Contact your local doctor if you experience:
- Redness around your wound
- Slowly increasing pain not controlled with your usual medicine
- Increasing swelling around the surgery area
- A bad smell or pus coming from the wound
- Broken stitches or opening wound
- Feeling hot, cold or feverish
- Constipation or trouble with bowel movements
- Anything that is worrying you or your family.
Call healthdirect Australia - 1800 022 222 if:
- Someone is sick and you are not sure what to do
- You need to know where to find after-hours health services or pharmacies
- You need advice.
healthdirect Australia is a 24-hour health advice line staffed by registered nurses to provide fast and simple expert advice on any health issue and what to do next.
Getting support
Being in hospital can be a difficult and stressful time. You may feel very anxious or have worries.
This is all part of adjusting to the changes that surgery and being in hospital can bring.
Some common worries you may have include:
- Doubt about the future and the outcomes that surgery may bring
- Feeling anxious, angry, frightened, depressed or confused about your surgery
- Worried about your family, home or work while in hospital
- Finding it hard to talk freely with your family or friends
- Confused about your situation
- Not knowing who can answer your questions.
Your family and friends are important to give you the emotional support during this time.
There are also a number of counselling and personal support services available – both while you are in hospital, and afterwards in the community.
Professional support
In hospital
Counselling and Personal Support services are available while you are in hospital. These include:
- Support to adjust after surgery
- Support with self-care (including family carers)
- Plans to manage anxiety and depression
- Referral to long-term counselling services
- Referral for legal advice
Social workers are available to provide free, confidential support when you are in hospital.
For example, when in hospital it is common to have lots of questions like:
- Can I get a Centrelink payment? How do I do that? Where can I go to get some financial aid?
- What community help is available to me?
- What accommodation options are available to me?
Social worker has information on these and more.
Talk to your nurse, who can arrange visits from these supportive professionals.
In the community
Psychology, social work and counselling services are also available in the community. You may wish to speak to someone before you come into hospital.
Giving support - for Carers
Your job as a supporter for a loved one in hospital for surgery, is a very important one!
How do I give the best support?
You know your loved one best, so you are in a perfect position to give them the emotional support that they need. It is important that they keep as calm, confident and positive during their hospital journey, as possible. That’s where you can help.
Knowing your loved one best also means you know when something is going wrong with them, and when to find help. As an advocator, you can make sure they get the care they need.
Listen carefully to the nursing staff, and don’t be afraid to ask questions if you don’t understand something. Even better – take notes. That way you can revisit them if you forget something, and make sure you and your loved one understand what is happening all the time.
Giving your loved one and the medical staff your full support and cooperation is also very important – this helps your loved one get the best care that they need.
Be sensitive
Make sure you listen to your loved one. This is obviously an anxious and worrying time for you, too. It helps to remind yourself that this is happening to them, and your job is to give them the type of support that they need. For example, some patients just want their supporters to listen.
It is important that you:
Stay objective – don’t try to filter out information you think they don’t want to hear. And try not to cloud things you say with your own feelings and opinions.
Stay calm – your mood will have a huge impact on your loved one!
Stay respectful – ask staff for help, instead of demanding it. Plus saying thank you is lovely and important for the caring staff, and for the mood of the patient.
Straight after surgery
Your loved one must have someone stay with them the night after surgery (if they are discharged home). If they have had a General Anaesthetic or sedation, they will need a responsible adult take them home and stay overnight. A small amount of anaesthetic may still be in their body, and their ability to do tasks may be affected.
They must not drive home after surgery – it is not safe.
If there is no-one to stay with and care for your loved one, please tell the hospital staff. We want them to have their surgery, but we also want them to be safe afterwards.
Caring for the Carers
Sometimes Carers need support too:
- For carer information, support and counselling contact Carers NSW between 9am to 5pm . Free call: 1800 242 636
- For carers needing emergency respite call: 1800 052 222
