Welcome to Shoalhaven Hospital Birth Unit!
Shoalhaven Hospital caters for all women who live in the Shoalhaven area and also visitors to the area.
Note: if you are visiting the Shoalhaven area we recommend you bring any pregnancy information in with you, including your antenatal record of care, which is most often a "yellow card".
Women booked in during their pregnancy through Shoalhaven Hospital or Milton Ulladulla Hospital will birth at Shoalhaven Hospital.
Women can birth at Shoalhaven Hospital from 36 weeks. Women who come to the hospital before 36 weeks and are in labour may be transferred to another hospital depending on the situation. Sometimes women are referred to another hospital for higher level of care if there are some issues that arise in pregnancy. The hospitals women are usually referred to are Wollongong Hospital and Royal Hospital for Women (Randwick).
Starting labour or have concerns?
Women who think they are starting labour or have concerns please:
- 20+ weeks - call Maternity or Birthing Unit
Maternity Ward Ph. 4423 9240
Birthing Unit Ph. 4423 9207
- Under 20 weeks – attend the Emergency Department.
Location
Our Birthing Unit and Maternity Ward (Postnatal/Antenatal) are located in the same place. They are on the same floor as the Hospital’s main entrance. After you enter the Hospital, turn right after entering the glass doors, follow signs to Maternity.
Note: Please ensure you follow COVID-19 screening procedures at the entrance to the hospital before coming to Maternity.
At Maternity there is a door-bell to press to alert staff of your arrival.
The Neonatal Unit is located next door, just a few metres away from the Birthing Unit.
This video shows you how to find your way.
Facilities
At Shoalhaven Hospital we have four Birthing rooms, each with a large bath. The Maternity Ward has 13 beds, some of these are single rooms, others are shared two-bed rooms.
Who can come to the birth with me?
You may bring a birth partner with you to hospital.
Due to COVID restrictions, that are often updated, please clarify the number of support people before you arrive by calling Maternity Ward ph. 4423 9240.
Please click here for Hospital Visiting Hours during COVID-19
If you are not in labour and need to stay overnight, we will ask your support person to go home overnight so everyone can get some rest, then they can return at 8am.
If you go into labour overnight your support person can be called to come back into the Birthing Unit.
What do I bring
From the 'Having a Baby' booklet (NSW Health)
For you:
• nightdresses or large t-shirts and a dressing gown
• some loose, comfortable day clothes
• comfortable footwear
• several pairs of comfortable underpants
• maternity bras and/or maternity singlets
• breast pads
• toiletries
• sanitary pads – either ‘super’ size or maternity size (you can buy maternity pads in supermarkets)
• something to wear while you’re in labour if you choose to wear clothes – a big T-shirt or an old nightdress, warm socks
• clothes for you to wear when you’re going home (you won’t be back to your normal shape yet and may still be in maternity clothes)
• anything you want with you in labour (e.g. music, massage oil, snack food).
For your baby:
• nappies and clothes for the baby to wear home
• cleaning products for baby, nappy wipes or cotton wool for baby’s nappy changes and soap or non-detergent wash for baby’s bath
• if you have a long distance to travel, you should also pack a change of clothes for the baby
• baby blanket
• baby capsule in your car.
Your partner or birth support person may also need to have a bag ready.
Think about:
• food and drinks for them during labour, as well as for you. This may include juices or other drinks,
soup, and foods that are easy to heat or ready to eat so they don’t have to leave you for long
• swimmers and towel (if you’re going to a hospital with a large bath, and you want support in the
water while you’re in labour)
• camera.
Am I in Labour?
Every labour and birth is different and varies depending when it starts and how long it takes.
Your midwife or doctor can answer any questions you might have about your labour and birth and what you and your partner can do to prepare.
There are three main stages of labour. The time taken for each stage will vary from woman to woman.
Everyone is different.
Stage 1 - when your cervix is opening
Stage 2 - when baby is being born
Stage 3 - when placenta is delivered
Have a look at p71 in this book for more information
 How will you know if you’re going into labour?
How will you know if you’re going into labour?
Most women experience one or more of these signs when labour is beginning:
• regular contractions/ period-like cramps
• a ‘show’
• waters breaking
Please call the BU if you think you are going into labour on Ph. 4423 9207
For more information, have a look at the "Having a baby book" given to you at the hospital or click here for an on-line version.
Upright and Active Birth
What is active birthing?
Active labour can help:
Promote shorter labour time:
By being active and upright in the first stage of labour women could shorten their length of labour by approximately one hour.
Make labour less painful:
Women who give birth lying down are more likely to have epidurals, but those labouring in an upright position are more likely to cope with the pain
It makes a more satisfying labour:
Being in an upright position women felt more satisfied with their birth experience overall and in control of their birth process for comfort positions.
Better oxygen for baby:
Being in an upright position allows for a better flow of blood to the baby. Lying down on your back can lead to a reduced flow of blood to the baby.
It makes the most of gravity:
It makes sense to utilise gravity during labour. Pushing in an upright position allows gravity to do its job and help the baby travel down through the birth canal.
Your partner will feel more involved in the birth process:
During an active labour, a birth partner feels like he or she is actively participating in supporting the mother-to-be. It also creates a rewarding and bonding experience for all.
Has the potential to result in less trauma to the baby:
Because an active birth can result in fewer interventions, less likelihood of stress to the baby or a longer than necessary labour. Of course, there are no guarantees, but active birth certainly helps to keep birth normal for both mother and baby.
Setting the scene for an Active Birth, please see the below picture to view some recommended labour birth positions.
What is the Perineum and how to protect it
The perineum (peh-ruh-nee-um) is the small area of tissue between the opening of your vagina and the opening of your back passage.
Why is it important to minimize or avoid causing perineal tears?
From this information leaflet, around 85% of women will have some perineal tearing during vaginal birth. This can cause pain and discomfort after birth.
For some women , sexual intercourse can become uncomfortable or painful for a short while. If this persists beyond 12 weeks it is important to see your doctor.
How can I avoid the damage?
Perineal massage can help reduce perineal tearing. Please speak to your midwife or doctor about this document on Antenatal Perineal Massage.
Pain relief options at Shoalhaven Birthing Unit
Understanding the choices of pain relief are an important part of getting ready for the birth of your baby.
Although having a baby is a natural process, every woman is different, and every birth experience is unique, so the need for pain relief varies.
There are different ways to manage pain during labour.
Available pain relief options in our Birthing Unit include:
-
Active birthing – mobility and birth props (Birthing Balls, peanut balls, birth mats)
-
Transcutaneous electrical nerve stimulation (TENS) – Woman supplies own TENS machine
-
Showers – Warm water (in every ensuite)
-
Baths- Water immersion for labour and birth (low risk women for birth). There is a large bath in all our birthing rooms.
-
Sterile water injections (SWIs)
-
Nitrous oxide (laughing gas)
-
Morphine (medicine])
-
Epidural (Patient Controlled Epidural Analgesia - PCEA)
Please click here for more in depth information on pain relief in the "Having a Baby" book.
Induction of Labour
If you have an Induction of Labour, your doctor or midwife will discuss all of the details with you as you will be asked to sign a consent.
An induction can be done in a couple of different ways. Your doctor or midwife will give you more information when they book a date for you (if required) and you will be provided with the information pamphlet below.
Shoalhaven Hospital Birth Unit phone 4423 9207
What is an Induction?
An induction of labour may be booked between 37 and 42 weeks of pregnancy.
Induction of labour usually involves medicine (oxytocin) combined with the breaking of waters in front of the baby’s head.
The lower part of your womb (cervix) is assessed to see whether it is ready for birth. Your doctor or midwife will talk to you more about this if you are having an induction of labour. You will receive an information leaflet and asked for your consent.
Checking the baby
Before and after we give you medicine for an induction of labour, we will check your baby’s heart beat with a device which records baby’s heart rate on paper (cardiotocograph: CTG) to make sure your baby is well.
You will be watched for:
- Having more than 5 period like cramps every 10 minutes, whilst you are being monitored.
- Having any stomach pain that feels quite painful (note: period like cramping is a side effect of the treatment).
- Broken waters without warning. If your waters do break on occasion this is not unusual.
- Any signs of too much bleeding ( a few blood spots after an internal examination is normal and expected).
- For any changes in your baby’s heart rate pattern
What things should make me alert a midwife or staff member whilst in hospital?
- If your baby’s movements reduced at any time, please alert staff
- If you have contractions or any other abdominal pain
- Broken waters, please note colour
- Any vaginal bleeding
- Unusual vaginal discharge
- Any other concerns or you feel unwell.
Prostin gel and Balloon catheters (tubes) have been used for cervical ripening consistently within maternity services and are considered safe for you and your baby. If you have any concerns regarding this treatment please discuss this with the doctor or the midwife.
Your Midwife will provide you with an information pamphlet on Induction of Labour
I'm having an elective Caesarean
Your doctor or midwife will talk to you about any risks and care during and after your caesarean.
When your caesarean is booked
- You will be given a date for your baby’s birth.
- The consent for the operation should be completed by a doctor.
- You will be given blood test forms and these tests need to be done the day before your operation
- Your midwife will also provide you with green antiseptic wash
The day before your caesarean
- Have the blood tests attended at Shoalhaven Hospital Pathology or Milton Ulladulla Hospital
- Call Maternity 4423 9240 after 3pm to confirm the time of your operation
On the day of your operation
- have a shower at home, using the green antiseptic wash. Please do not wash your breasts or chest with the antiseptic wash, wash from under your breasts downwards
- Please remove all makeup, nail polish and jewellery before coming to the hospital.
Fasting
- If you are having a morning operation (8am) you must not eat or drink from midnight. You come to the Maternity Unit at 6am.
- If you are having an afternoon operation (1pm) you must not eat or drink from 6am. You come to the Maternity Unit at 10am.
- Gestational Diabetes / Diabetes - your diabetes educator, endocrinologist, doctor or midwife will talk to you about your tablets or insulin before your operation.
Arriving on the Maternity Ward
- Your blood pressure, pulse, temperature, baby’s position and heart beat will be checked.
- The area near your bikini line will be clipped. Please do not to shave or wax this area in the 10 days before your operation because of the increased risk of wound infection
- You will then get dressed in a hospital gown, be measured for special compression stockings for your legs, identification bands will be applied and you will be asked a series of questions by the midwives in preparation for your operation.
- Then you wait for your turn in the operating theatre and will return to the same room.
- Your support person will be supplied with scrubs to wear in theatre [please wear closed in shoes]
What to bring
- Check the list of what to bring to hospital when packing your bag.
- Remember your camera or phone and charger.
Support people
- A single support person can accompany you to theatre and be with you if you are awake for the caesarean. Although it is exciting it may be better to let other friends and relatives know after the baby is born and you have had a chance to feed and cuddle your baby.
- It may take up to 2 hours before you are back on the Maternity Ward after having your baby.
- Your partner may come in earlier at 8am-8pm. We recommend limiting visiting on the first day.
- Visiting may be affected by COVID restriction. Please contact the Maternity Ward as close to your birth as possible to find out the most recent updates.
After your baby is born
The midwife that accompanies you to theatre will assist with taking photos, feeding and encouraging skin to skin contact. Your baby will be weighed and measured. Staff will ask for your consent for Vitamin K and the Hepatitis B vaccines for your baby.
General post operative information
- You will have a drip in your arm until you are drinking well.
- You will have a catheter draining your urine until you are able to get to the bathroom.
- You will have ‘calf compressors’ on that reduce the risk of clots occurring in your legs after an operation.
- Your stockings will still be on. These should be used for 6 weeks after your operation.
- You will be encouraged to take regular pain relief. This helps you in the first few days after you major surgery and helps you to care for your baby.
- You will be assisted to feed and care for your baby.
- You will be helped to shower 8 – 12hours after your operation.
Looking after your wound
- You will have a waterproof dressing over your wound. However, if your wound dressing is coming off even a small amount, please let staff know as the dressing may need to be changed.
- Some doctors like to use a stitch that needs to be removed. The MAPS midwife will continue wound care after discharge from hospital.
- To reduce the risk of infection it is important to;
- Use the hand wash before and after nappy changes and encourage others before touching your wound or your baby to do the same.
- Shower three times day with a skin friendly soap allowing the water to run over your wound.
- Do not rub or scrub your wound, be gentle and pat dry with a clean towel.
- Place a dry clean pad between your wound and underwear and change any time it falls out or any time you go to the bathroom.
- Do not use powders, creams or gels on this area
Reducing the risk of wound infection
After the dressing is removed, it is important to look at your wound regularly for signs of infection.
This includes signs of redness, swelling, discharge or ooze, increased pain or you have general feelings of being unwell.
Looking after yourself
- Normal healing takes up to 6-12 weeks so be careful twisting, lifting, stretching or with any sudden movements. You will be able to care for your new baby.
- Try to eat well, get plenty of rest and accept any help that is offered.
- Adjusting to parenthood is exciting and challenging. Be kind to yourself.
- Arrange follow up with your doctor at your 6 week postnatal check.
- Remember there is support for you in the community. Child and Family community-based services provided throughout the ISLHD include: Child and Family Health Nursing clinics and home visits, Allied Health and Diagnostic Assessment specialities, in addition to Aboriginal, maternal infant and child services and family care centres, child protection and wellbeing, and a variety of groups across the services. Interpreters are available free of charge as required.
Good luck and enjoy this amazing journey.
Tips before baby arrives - e.g. capsule
New parents have found doing these before your baby arrives can make a big difference:
- plan a date night before baby arrives
- learn about breastfeeding - click here
- prepare and freeze meals
- finish any projects around the house
- take a hospital tour and book into childbirth education classes
- stock up on groceries and other supplies (don’t forget sanitary pads)
- organise a baby capsule- All babies must travel in a baby capsule or restraint in the car. You can hire a capsule or restraint or you can buy one. For more information about baby capsules and car restraints for children, click here or search at www.rms.gov.au
- know what's normal for babies - see Raising Children
- put phone numbers of your support people in your phone or on your fridge for the grandparents, for example Australian Breastfeeding Association counsellors - 1800 mum2mum, the number for your GP
Going home from Birthing Unit
Speak to the midwife looking after you if you plan to go home from the Birthing Unit. You will be required to stay at least 4 hours after birth.
Vaccinations for baby
With your consent, at birth, your baby will receive their Hepatitis B vaccination and Vitamin K injections.
Click here for more information about Hepatitis B vaccine
Click here for more information about the Vitamin K injection
After-birth support
Our friendly midwives and doctors help new parents with getting to know their new baby while in hospital and also put families in touch with further support for when they go home.
R.E.A.C.H. out to us
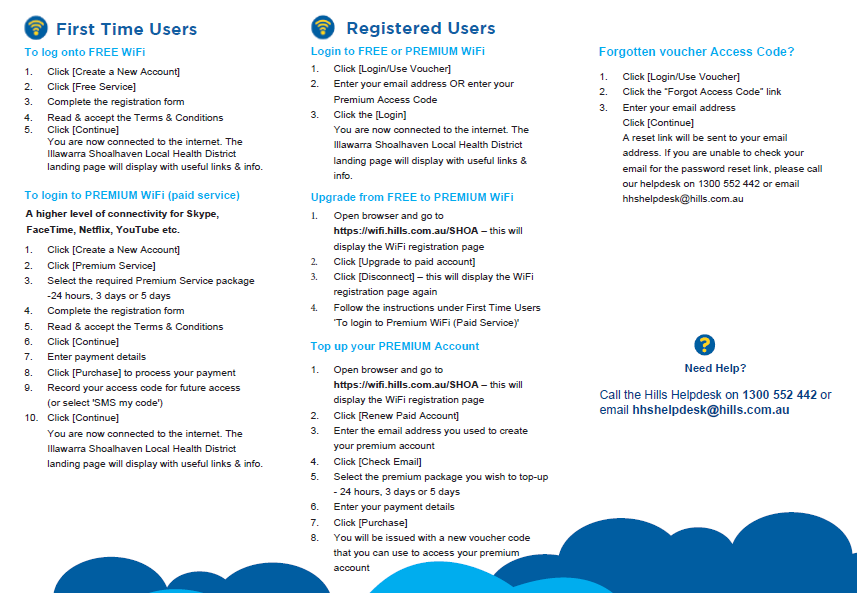
Wi Fi

Need an Interpreter? Professional interpreters are available if you need help to communicate with staff. Our staff can also ask for an interpreter. The service is free and confidential. We will book the interpreter for you. You can also call the Translating and Interpreting Service on 131 450 if you need to speak to us before your appointment. Click here for more information about the Illawarra Health Care Interpreter Service.
