Welcome to Shoalhaven Hospital! Congratulations on your pregnancy or new baby!
Our Maternity Ward provides woman centred care for women and their families in the Shoalhaven Region.
The Maternity Ward is located in the same ward as the Birthing Unit, and just a few metres away from the Neonatal Unit.
The Maternity Ward has 13 beds, some of these are single rooms, others are shared 2 bedded rooms.
Discharge planning is discussed with the midwife providing care and the average length of stay is 48 hours.
Shoalhaven Hospital offers a home visiting program that supports your care in your own home provided by your team of MAPS (Midwifery Antenatal Postnatal Service) Midwives who provided you care while you were pregnant.
Visiting Hours: Please call the Maternity Ward for visiting hours and amount of visitors allowed. Due to changing COVID restrictions these are often updated.
Please click here for our visiting hours as they may change with COVID restrictions
Maternity Ward ph. 4423 9240
How to get to Maternity at Shoalhaven Hospital
What to bring to hospital
From the 'Having a Baby' booklet (NSW Health)
For you:
- phone charger (labelled) and phone
- loose, comfortable day clothes and pyjamas
- comfortable footwear
- comfortable underpants (high waisted preferable)
- maternity bras and/or maternity singlets
- breast pads
- toiletries
- sanitary pads – either ‘super’ size or 'maternity' size (you can buy maternity pads in supermarkets)
- loose change for vending machines
- water bottle
- pen to write feeds down
For your baby:
- nappies and clothes for baby to wear
- cleaning products for baby, nappy wipes or cotton wool for baby’s nappy changes and soap or non-detergent wash for baby’s bath
- if you have a long distance to travel, you should also pack a change of clothes for the baby
- baby blanket (labelled)
- bibs and washcloths (labelled)
- baby capsule in your car
Length of Stay in Hospital
Depending on the type of birth you have and how you and your baby are feeling, you would stay at least four hours after the birth and possibly up to three days.
Every woman, birth and baby are different, please talk to the Midwife caring for you, about planning to go home.
Discharge from the ward
Mother
When you are discharged you will be supported by the MAPS team that supported you during your pregnancy. MAPS may be able to visit you in your home to help with breastfeeding and infant care. Check whether you are eligible for a home visit by speaking to your midwife on the ward.
If we cannot visit you at home, we can arrange a visit with the MAPS midwife at the Maternity Ward. If you are discharged before your baby has a hearing screen (State Wide Hearing Screen), you will be contacted and the hearing test can be attended on the ward.
You may need to make an appointment for a 1 to 6 week check-up with your GP (doctor). Check with the Midwife caring for you when this appointment is needed.
Baby
Before you go home your baby will have a physical check-up before you go home by the midwife or paediatric team on the ward. You will be asked to book an appointment with your GP (doctor) for another check-up for baby 7-14 days from baby's birth.
Who will support me when I go home?
The MAPS team that supported you during your pregnancy will see you after you are discharged from the hospital.
This may be done at your home, there are times that we may not be able to visit you and you may be asked to return to the Maternity Ward to meet the MAPS midwife.
Home visiting is usually available if you live between Gerringong - North Durras.
What can you expect from these visits?
We offer midwifery services with a combination of home visits, phone calls and no contact days. Your midwife will usually visit sometime between 8.30 am - 3.30 pm. If you are not available, please phone your midwife before 9am to cancel your visit for that day.
The MAPS team will help you gain confidence in feeding and parenting skills. We will also weigh your baby and do checks on you and your baby. Most midwifery care you received in hospital can also be provided when you go home.
Your individual needs will be assessed at each visit. The service finishes by mutual agreement usually when your baby is day 5-10, but the service is available until day 14.
Child and Family Services and/or your GP will also support you after you go home.
Safety for the Midwife
Before you are discharged from the hospital we will do a checklist to ensure your home is safe for the midwives to visit, including pets, renovations etc. If any safety issues arise we may be unable to visit you at home, but will offer you a visit at the Maternity Ward.
We request that all family pets should be secured during the midwives visit.
Is there a fee?
These postnatal visits are free to Medicare card holders.
Please note, if you are not eligble for Medicare, each visit and any related service such as interpreters and pathology will be charged separately.
MAPS team contact numbers
Shoalhaven MAPS
Ph: 0411 402 441
Ph: 0448 483 809
Milton MAPS
Ph: 0417 671 953
Ph: 0436 357 434
Looking after yourself after birth
Your uterus (womb) - It takes a few weeks for your uterus to get back to normal. It happens faster when you breastfeed.
Cramps - You may feel some cramps as your uterus contracts down to its normal size. They can be more noticeable when the baby is sucking. Some women find that the ‘after-birth pains’ are more painful after a second baby or more.
Bleeding from the vagina is normal for up to 3-4 weeks. The first 12-24 hours after birth may be heavier than a normal period. Eventually it will lessen to a brownish discharge. Use pads as tampons are not recommended. Change them every time you go to the toilet.
Your perineum (bottom) - sitting down can be uncomfortable, especially if you have stitches. These dissolve so you don’t need to have them removed. Midwives will check the area to make sure it’s healing normally. Keep it clean and dry by washing 2-3 times a day and after going to the toilet.
Pain relief - try lying down and resting to take pressure off your perineum (bottom). You can use paracetamol if needed (if you are at home please follow directions on the pack or if you are on the ward, ask your midwife). There is a brochure below that might help for more information.
Breasts - All women produce breastmilk. This usually starts around 16 weeks of pregnancy and you may have been leaking. For the first few days after birth, breasts are soft because your baby only needs a very small amount of breastmilk. Once babies start to get hungry and feed more frequently, the breasts respond by producing more milk. Your breasts may feel fuller and heavier as your milk ‘comes in’.
Please click here for more information about feeding your baby
Caesarean section - if you had a caesarean operation, your scar is usually a low horizontal cut on your tummy, below your bikini line. Dissolving stiches are generally used these days which means the stitches don’t need to be removed. The scar can be sore and uncomfortable for a few weeks. You’ll be given pain killers in the first few days to help ease the pain as you gently and slowly move around and care for your baby.
'Rooming In' - Having your baby stay with you in your hospital room will help you get to know each other and support breastfeeding. Our staff are here to help you learn to care for baby when you go home and this is a great opportunity to ask for help.
Your feelings - You may feel sensitive, weepy and a little cranky. Most women go through this for a few days after the birth or even up to 2 weeks. If these feelings last longer than this, talk to your midwife, early childhood nurse or doctor (GP).
Resources
- ISLHD Child and Family Services (Kids and Families page)
- This information is from the NSW Health "Having a baby booklet", click here for the whole book
Postnatal exercises
Postnatal Exercises
Healing after birth takes time so try to balance your rest and activity.
Click here for more information about recovery after birth (Raising Children)
Pelvic floor exercises -
Why exercise the pelvic floor?
Leaking can really impact how you live and stop you from doing things that you enjoy. A healthy pelvic floor can help with many types of leaking, minimise back pain and keep you moving well. This will take just 5 minutes a day.
Finding the right muscles
The pelvic floor is a deep group of muscles at the base or “floor” of the pelvis. Most women describe doing a pelvic floor exercise as a squeeze in and a lift up of the muscles around the vagina and back passage.
How many should I do?
Here is a routine to aim for that is easy to remember. Consistency is the key so it’s a good idea to set an alarm every day until you get into the habit. The long holds will help with your endurance; the strong holds are important for supporting your bladder and back when you cough, sneeze or exercise.
Start with less and build up to:
- 10 LONG holds (gently squeeze and hold up to 1-2 seconds, before letting go – gradually work up to a 10 seconds)
- 5 STRONG holds (squeeze up and in as hard as you can and then let go. Gradually build up to 10 strong holds)
Rest a minute or so and then repeat 2 times, rest for a minute or so and repeat 2 more times.
Looking after yourself
Click here for some resources for looking after yourself when you have a new baby
Wound care after a Caesarean birth
Wound care and looking after yourself is important if you have a caesarean birth. The wound dressing will stay in place from 5 to 7 days as per the doctors instructions.
Personal care
- Always wash your hands with soap and water after tending to baby
- Shower at least once a day, allowing water to run over wound dressing or clean wound.
- Pat wound with clean bath towel when dressing has been taken down.
- Do not use any creams or powders on wound area once the dressing has been removed.
- You might find a pair of full brief underpants more comfortable than bikini briefs as they may rub the operation area.
Look for signs of infection:
It is important to talk with your midwife, nurse or doctor if you feel you are experiencing any signs of infection
Signs of infection include:
- Redness
- Odour
- Swelling
- Discharge from the wound
- Increased pain
- Temperature (high or low) or feeling unwell
Healing
- Normal wound healing on the top of the skin will occur in the first week
- The underlying layers can take up to 6 weeks to heal
- You will gradually feel like you are able to do more activity. Take care when twisting, stretching, bending, lifting baby or sudden movements.
Over the next 6 weeks it is advised that you:
- avoid lifting or pushing anything that causes you pain
- avoid soaking in bath or swimming until your wound has healed
- avoid driving your car until you are able to use pedals quickly and without pain (see your car insurance requirements)
- enjoy gentle exercise that does not cause any pain around your wound
- rest when you are tired
Recovery after caesarean section- click here for more information from 'Raising Children'
Feeding your baby
The first breastfeed (newborn baby in birthing unit)
As a newborn, most breastfeeding sessions may be 15 minutes, 45 minutes or even longer. Most babies are quite awake when they are first born and this is the best time to do skin to skin and look for baby's feeding cues before breastfeeding. Every baby is different .
Some, babies will then want to feed every hour, 2 hours or up to 6 hours later. Some babies will feed from both breasts or just one until they are satisfied. Let your baby feed 'on demand' (when they look hungry) and offer skin to skin if baby does not want to feed at that time.
Click here for Australian Breastfeeding Association information on the early days of breastfeeding
ABA - breastfeeding cues - know when baby says 'I'm hungry'
Breastfeeding (click here for our 'feeding your baby' page)
The more your baby feeds at your breast, the quicker your milk supply will build. You may feel your milk 'come in' (breasts feel full) from 2-5 days from baby's birth. It is very important to feed baby when they are hungry (on demand), not by the time they were last fed. Sometimes baby will be satisfied after a short feed, other times baby will want to feed longer at the breast (up to an hour).
"Cluster" Feeding
It is normal for babies to feed close together and frequently. This is called "cluster feeding". This can occur when baby is newborn or during growth spurts (times when baby grows and is very hungry). It is normal for babies to feed 2-3 times through the night. Look out for early hunger cues (rooting, smacking lips, and more) and offer the breast straight away.
Is my baby getting enough?
You know if your baby is drinking plenty of milk when he/she:
- Has good skin colour and muscle tone and looks bright and alert when awake
- Has at least 6 pale, wet cloth nappies (or 5 disposable nappies) in 24 hours (when milk is in - this is often after day 4).
- Wee's (urine) should look clear and pale. If dark
- A young breastfed baby usually has 3 or more soft runny poos on most days, mostly yellow in colour. If it looks like toothpaste or is hard, see your doctor.
- Some weight gain (you can look at baby's growth charts in the 'Blue Book' after birth and visit your GP or Child & Family nurse for accurate weight measurements)
- more information available here (ABA)
For further information:
Breastfeeding Your Baby booklet (NSW Health)
Australian Breastfeeding Association
ISLHD Child and Family Services
Raising Children Network videos
Download the Milky Way Breastfeeding App on your phone:
Normal Newborn behaviour
Remember that all babies are different and the information below is a guide only. If you have any concerns talk with your doctor, early childhood nurse or midwife.
Behaviour
Cuddling, sleeping, feeding. That’s what it’s all about in the first few months.
Your baby is learning a lot as you spend time together every day. Their brain grows and develops as they see, hear and touch the world around them.
Your baby might be able to follow your face with their eyes. Around this age faces are the most interesting thing to baby. They will also like to look at toys with contrasting colours, for example, red, black and white. Your baby will enjoy toys with faces or patterns like swirls or checks.
Your baby can hear you and knows your voice, but might sometimes startle when they hear you or another sound.
Eye contact is one way your baby tells you they want your attention, but they communicate mostly through crying.
Baby might lift their head briefly when lying on their tummy or turn to the side when lying on their back. This helps to see where you are and what’s around them.
(Raising Children Website, NSW health)
Tests for baby in hospital
NSW Newborn Hearing Test

All babies in NSW are offered a Hearing (SWISH) Program screen. Since 2002 over 95% of babies born in NSW have been screened.
The hearing screen is done when baby is asleep and settled. It helps identify babies that could have permanent hearing loss. The hearing screener will ask for your consent before baby is screened. Please Click here for more information.
NSW /ACT Newborn Screening Test
Newborn screening tests are offered to all babies born in NSW and the ACT. A blood sample is collected from the heel of babies onto a pre-printed filter paper card. Collection occurs in our maternity ward or at home by our midwife support program.
Please click here for more information.
Vaccinations
With your consent, at birth, your baby will receive their Hepatitis B vaccination and Vitamin K injections.
Click here for more information about Hepatitis B vaccine
Click here for more information about the Vitamin K injection
Nutrition for mum after after your baby is born
Choose a wide variety of foods from all food groups. Focus on filling up from healthy resources:
- protein
- fruit
- vegetables
- fibre-rich carbs
- fats like avocados, nuts and seeds.
- drink to thirst
Every woman's diet needs are different and depend on many factors. If you do have a health condition such as diabetes, your dietary plan may be different to ensure blood glucose levels are stable.
Please click here for more information:
R.E.A.C.H out to us
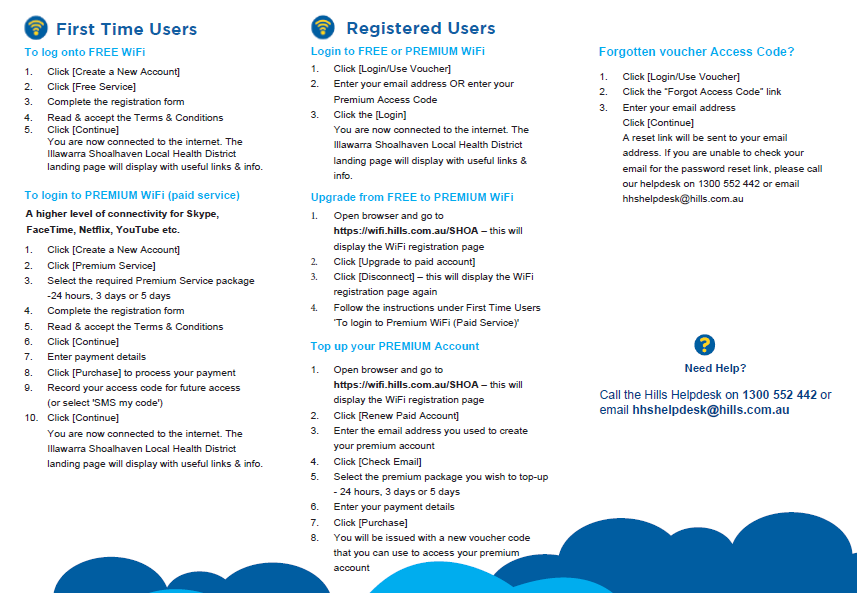
WiFi

Need an Interpreter? Professional interpreters are available if you need help to communicate with staff. Our staff can also ask for an interpreter. The service is free and confidential. We will book the interpreter for you. You can also call the Translating and Interpreting Service on 131 450 if you need to speak to us before your appointment. Click here for more information about the Illawarra Health Care Interpreter Service.
