
This web page will provide some information to guide you through a few questions you may already have.
Please ask us at your visits if you don’t understand or need some more information.
If you or your loved one has experienced or is experiencing HG, we welcome you to share your story and provide feedback on your experience to help us improve our service.
To connect with our HG Nurse, please click here to send your name, and contact details
What’s the difference between NVP and Hyperemesis Gravidarum?

Nausea and vomiting in pregnancy is generally defined as symptoms of nausea, vomiting and/or dry-retching commencing in the first trimester without another cause.
It is estimated to affect around 69% of pregnancies and often resolves after the first trimester.
Hyperemesis Gravidarum is defined by the following features:
-
Symptoms start in early pregnancy, before a gestational age of 16 weeks
-
Characterised by severe nausea and/or vomiting
-
Inability to eat and/or drink normally
-
Strongly limits daily activities
-
Some women may show signs of dehydration and/or electrolyte abnormalities
What happens if I have HG?
If you suspect you have HG, make an appointment to see your care provider as soon as possible.
At your appointment they will assess you utilising the PUQE-24 tool. You may also require further testing to exclude other possible causes of nausea and vomiting.
If you are diagnosed with HG, your care provider will create an individualised care plan to treat and alleviate your symptoms. This could include a combination of lifestyle changes and medications. It is important to note that your care plan may need to be changed and updated, if you are not experiencing any relief of symptoms return to your care provider so they can try a new option.
How is NVP and Hyperemesis Gravidarum in pregnancy diagnosed?
It is recommended that all women are asked about nausea and vomiting in pregnancy at each pregnancy visit between 4-16 weeks gestation. If nausea and vomiting is present, your care provider will use the PUQE-24 to classify your severity of symptoms, this includes your weight loss and hydration status. PUQE-24 is a validated scoring system to classify the severity of nausea and vomiting in pregnancy. The PUQE-24 scoring system assesses the severity of nausea and vomiting over a 24 hour period, with three questions relating to duration of nausea, frequency of vomiting and dry retching symptoms. An additional question considers overall wellbeing in the previous 24 hours.
What help is available to me?
Treatment options and advice need to be based on your individual symptoms and severity.
Development of local care pathways is recommended to support consistency in assessment, diagnosis, management and treatment. An individualised management plan held by you and provided to the multi-disciplinary team is required to support coordinated and continuous care. The management plan will include advice on how to adjust care if symptoms improve, fluctuate or deteriorate and how to access care if required.
The below link is for a care plan you can start to fill out for discussion with your care provider.
Link to My Sickness in Pregnancy Plan
The Non-pharmacological interventions for nausea and vomiting in pregnancy will be dependent on your symptoms and their severity. Interventions may include:
-
modifying activity to gain more rest or bringing forward bedtime
-
changing dietary habits to maintain hydration and nutrition (i.e. small amounts of well-tolerated food)
-
oral ginger and/or pyridoxine (vitamin B6)
-
acupressure bands
-
avoid iron-containing preparations
-
Psychosocial support.
In regards to Pharmacological treatments, this will need to be discussed with your primary care provider.
If you are suffering from dehydration and electrolyte imbalance your care provider may consider the use of intravenous fluids. Intravenous fluid and electrolyte replacement is an effective treatment for dehydration, electrolyte imbalance and nausea and vomiting and are valuable for both outpatient and inpatient management of the symptoms.

Support Options
Below is a list of external organisations that can help when you are trying to navigate HG. You may like to have family and friends check them out so they can have a bit more understanding of what you are going through. Please click on the images below to go to the websites.
 |
Hyperemesis Australia is a nation-wide charitable organisation focussed on supporting sufferers of pregnancy sickness, their families and healthcare professionals. Hyperemesis Gravidarum is an under-diagnosed and misunderstood condition and it is our mission to change this. No one should have to suffer in silence or receive inadequate care and we are here to support you during this difficult time. |
 |
The HER Foundation is the global voice of HG. Each year, millions of women with HG across the globe experience trauma, financial strain, debility and/or incredible misery due to severe nausea and vomiting of pregnancy (Hyperemesis or HG). HER Foundation empowers those managing HG with information and support to minimize suffering, long-term health complications, and pregnancy loss. |
 |
Centre of Perinatal Excellence (COPE) is a not for profit organisation devoted to reducing the impacts of emotional and mental health problems in the pre and postnatal periods. |
 |
PANDA – Perinatal Anxiety & Depression Australia supports women, men and families across Australia affected by anxiety and depression during pregnancy and in the first year of parenthood. PANDA operates Australia’s only National Helpline for individuals and their families to recover from perinatal anxiety and depression, a serious illness that affects up to one in five expecting or new mums and one in ten expecting or new dads. |
 |
MothersafePhone number 1800 647 848 MotherSafe is a free telephone service for the women of NSW, based at the Royal Hospital for Women, Randwick. About MotherSafeMotherSafe provides a comprehensive counselling service for women and their healthcare providers concerned about exposures during pregnancy and breastfeeding. Such exposures may include:
Mothersafe Nausea and Vomiting Factsheet |
Complications to be aware of
Complications of uncontrolled hyperemesis gravidarum can include:
-
malnutrition and loss of muscle mass, women with hyperemesis will frequently lose at least 5% of their pre pregnancy weight
-
Mallory-Weiss tears, constant vomiting can result in tears to oesophagus
-
hyponatremia and hypokalaemia
-
venous thromboembolism
-
abnormal thyroid and liver function
-
placental dysfunction associated with an increased risk of small for gestational age babies or preterm birth, preeclampsia and an increased risk of placental abruption
-
dehydration and renal failure
-
haemorrhoids
-
alterations in mental health status and impact on the family unit
-
dental enamel erosion, see attached reference for patient education on maintaining oral hygiene when consistently vomiting. Many women will want to freshen their mouths following vomiting however the constant brushing can damage the enamel.
| Keep Smiling While You Are Pregnant | Healthy Smiles | Keep Smiling While You Are Pregnant |
| English | for Aboriginal women | Other Languages [Arabic, Chinese, Khmer, Vietnamese] |
 |
 |
What happens after baby is born? Postnatal care
Postnatal Care and Transition to Child and Family Health Services, Primary Health and or General Practice
Nausea and vomiting in pregnancy or hyperemesis gravidarum often impact women’s psychological and emotional wellbeing and family unit. Women who experience these conditions are more likely to describe high levels of post-traumatic stress syndrome and associated negative outcomes.
It is recommended that postnatal care plans are developed in partnership with the woman during pregnancy to ensure a seamless transfer of care from maternity to community-based services, such as Child and Family Health services and General Practice. For Aboriginal families refer to Aboriginal Child and Family Health services.

Will HG affect my baby?
Your baby may be affected if you become very ill with untreated dehydration.
If this happens your baby may be born with a low birth weight.
However, not all babies born to women with hyperemesis gravidarum have a low birth weight.

Planning for the next pregnancy
Women who have experienced Hyperemesis Gravidarum in a previous pregnancy will benefit from pre conception support, counselling and early or pre-emptive treatment with antiemetic therapy.
-
High risk of recurrence of NVP and HG in subsequent pregnancies.
-
Suspect the risk is underestimated as women with severe symptoms may be unwilling to consider further pregnancies.
-
Pre conception support is highly beneficial.
-
Subsequent pregnancies should be seen as early as possible in the first trimester.

HG Myths & Facts
Having HG can feel extremely lonely especially when those closest to you don’t really understand what’s going on. Below are some of the mistruths people may say to you, but it’s really important that you focus on the facts. A table of the differences in which morning sickness and Hyperemesis Gravidarum affect women is provided for reference.
MYTHS
-
HG is the same as morning sickness.
-
You’re making a big deal out of nothing.
-
My mum vomited when she was pregnant and she’s fine.
-
It can’t be that bad.
-
You’re weak. You just need to toughen up.
FACTS
Hyperemesis Gravidarum is a significant debilitating illness affecting both the physical and mental aspects of women’s lives.
If you get anything out of this website it should be to feel validated you don’t have to try and just carry on, what you are going through is incredibly hard, you are entitled to supportive care and treatment.
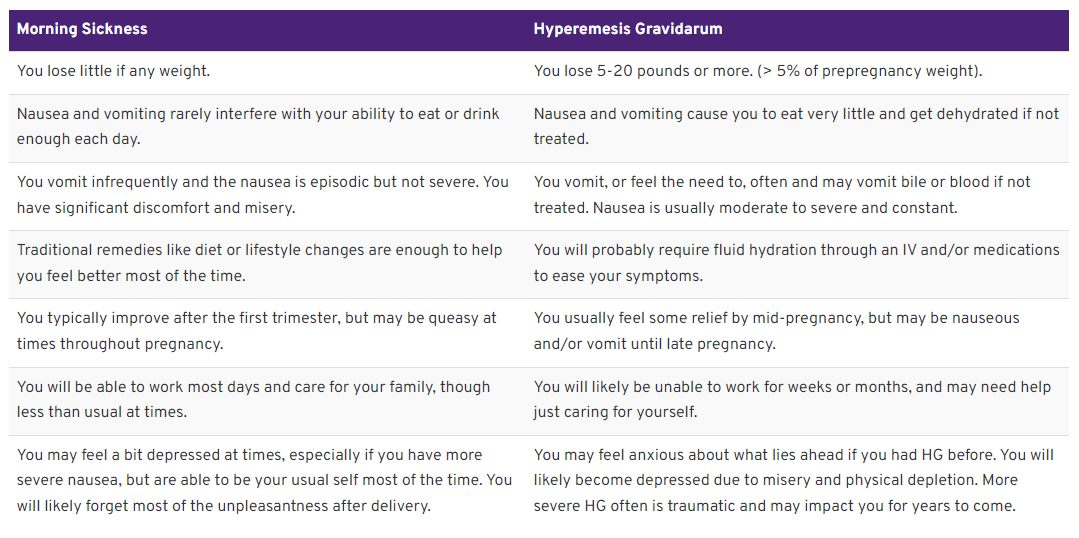
Image: HER Foundation – Available from: HER Foundation - Do I Have Morning Sickness or HG? (hyperemesis.org)
Key Concepts
-
Hyperemesis Gravidarum is a significant debilitating illness affecting both the physical and mental aspects of women’s lives.
-
Seek treatment early. Initiating an appropriate care plan earlier will vastly improve outcomes.
-
Assessment utilising the PUQE-24 scoring system.
-
Seek additional supports
-
Discuss with your care provider to ensure postnatal care is arranged

Resources
Need an Interpreter? Professional interpreters are available if you need help to communicate with staff. Our staff can also ask for an interpreter. The service is free and confidential. We will book the interpreter for you. You can also call the Translating and Interpreting Service on 131 450 if you need to speak to us before your appointment. Click here for more information about the Illawarra Health Care Interpreter Service.
